
HT5. Does the Color of the Pens Affect Male Health?
Why Skin Color in This Area Matters
The appearance of the skin—especially its color—can be a powerful indicator of what’s going on beneath the surface. Just like with other parts of the body, changes in the color of the pen*s may reflect anything from normal variations to signs of underlying health issues. While some differences in tone are harmless, others may require attention.
Understanding what’s normal, what’s not, and when to see a doctor can help you take better care of your intimate health without embarrassment or confusion.
1. Normal Color Variations

It’s completely natural for the pen*s to be darker than the rest of the body. This area tends to have more pigmentation due to hormonal sensitivity and skin thickness.
Common and Harmless Differences:
-
A slightly darker shade of brown or red-brown is normal, especially for individuals with darker skin tones.
-
Visible veins or mild marbling under the skin can be normal due to thinner dermal layers.
-
The head of the pen*s (or gl*ns) may have a pink or purple hue when blood flow increases during arousal or temperature changes.
As long as these colors remain consistent and aren’t accompanied by pain, discharge, or texture changes, they are generally considered healthy.
2. Sudden Redness or Inflammation

While a flushed appearance after physical activity or intimacy is common, persistent redness may suggest irritation or infection.
Potential Causes:
-
Allergic reaction: From soaps, detergents, or lubricants.
-
Inflammation (balanitis): Often related to poor hygiene, tight skin, or microbial imbalance.
-
Fungal or yeast infections: Can cause red, itchy patches with white residue.
Keeping the area clean, dry, and free from harsh chemicals helps prevent irritation. Consult a provider if symptoms last longer than a few days.
3. Purple or Blue Discoloration
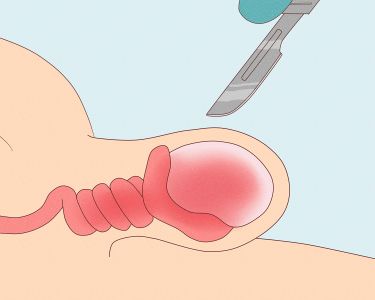
Temporary bluish color may appear when blood flow is restricted—like during cold weather or physical pressure. However, if the pen*s remains purple or feels numb or painful, it could signal something more serious.
When to Worry:
-
Circulatory blockage
-
Injury or trauma to blood vessels
-
Blood clotting disorder
Seek urgent care if the color does not return to normal within a few hours or is accompanied by swelling or loss of sensation.
4. White or Pale Appearance

A paler tone may occur when there’s less blood flow or exposure to cold. However, white patches or flaky skin may suggest a dermatological condition.
Possible Causes:
-
Vitiligo: A harmless autoimmune skin disorder causing depigmented patches.
-
Lichen sclerosus: Can cause white, thin skin and discomfort.
-
Fungal infections: Often accompanied by itching or odor.
These conditions are usually treatable but should be diagnosed by a dermatologist or urologist.
5. Yellow or Green Tint
Discoloration in these shades is uncommon and usually a red flag for infection or poor hygiene.
What It Might Mean:
-
Pus or discharge from bacterial or transmitted infections
-
Skin infection with surface crusting or odor
-
Contact dermatitis from irritating fabrics or products
Any yellow or green discoloration, especially if accompanied by fluid or foul smell, requires medical evaluation.
6. Dark Spots or Patches
Occasional small dark moles or freckles are often benign, especially if unchanged for years. However, new or changing spots should always be assessed.
When to Check for Warning Signs:

-
Spot grows in size or changes shape
-
Color becomes irregular (black, blue, or bleeding)
-
Appears raised or rough with unclear borders
These could indicate skin cancer or precancerous changes, and early detection greatly improves outcomes.
How to Keep Skin Tone in This Area Healthy

1. Practice Gentle Hygiene
Use unscented, mild soap and warm water to clean. Avoid over-washing or scrubbing harshly, which can irritate the sensitive skin.
2. Wear Breathable Fabrics
Loose-fitting underwear made of cotton helps minimize sweat, friction, and heat buildup—reducing risk of rashes or infections.
3. Stay Hydrated and Eat Well
Nutrient-rich diets with antioxidants can help maintain skin health. Vitamins C and E are especially important for skin tone and healing.
4. Limit Chemical Exposure
Avoid perfumed lotions, dyes, or aggressive grooming products that may trigger allergic reactions or pigmentation changes.
5. Monitor for Changes
Check your lower body skin tone regularly, especially after using new products or during seasonal changes. Catching new symptoms early leads to better outcomes.
When to See a Doctor
Contact a healthcare provider if you notice:
-
New discoloration that spreads or darkens
-
Persistent redness, white patches, or flaking
-
Pain, itching, or fluid discharge
-
Skin thickening, rough texture, or bleeding lesions
These symptoms can stem from infections, allergic reactions, or underlying conditions requiring medical attention.
Final Thoughts
The color of your pen*s can tell you a lot about your health. While many shades and patterns are perfectly normal, sudden or persistent changes may point to infection, inflammation, or circulation issues. Don’t panic—but do stay informed. By maintaining hygiene, observing changes, and seeking care when needed, you can stay ahead of any concerns and protect your long-term wellness.
Sources:
-
Mayo Clinic – Male Genital Skin Disorders
-
Harvard Health – Dermatology and Skin Care
-
CDC – Infections and Prevention
-
American Academy of Dermatology – Vitiligo & Lichen Sclerosus
-
Johns Hopkins Medicine – Urology and Skin Lesions



